BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://nmj.umsha.ac.ir/article-1-2014-en.html
2- Department of Medical Surgical Nursing, School of Nursing and Midwifery; Student Research Committee, Rafsanjan University of Medical sciences, Rafsanjan, Iran
3- Department of Radiology, school of Paramedicine, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
4- Department of Community Health Nursing, School of Nursing and Midwifery; Social Determinants of Health Research Center, Rafsanjan University of Medical science, Rafsanjan, Iran ,
✅ The presence of family members and their training before presence did not reduce the anxiety of patients under nursing invasive procedures. It's necessary that other aspects of family members’ presence during invasive procedures to be considered in future studies.
In most patients, hospitalization is associated with varying levels of stress and anxiety [1]. Anxiety as a predictor of mortality and morbidity can be associated with an increase in negative outcomes [4-6]. In addition to common pharmaceutical methods, researchers have proposed several procedures for managing anxiety in patients, including family-based approaches [10]. Nowadays, the presence of family members in critical situations on the bedside of patients has become a challenging issue. Most families tend to be with their loved ones during critical events and aggressive procedures [14]. Health system staff also have mixed views on this issue [15–17], but little is known about adult patients' perceptions of family members presenting during emergency care and unscheduled aggressive procedures. Therefore, this study was designed to determine the effect of pre-family training and attendance on anxiety level of patients undergoing aggressive nursing procedures admitted in emergency department.
In this clinical trial study, 90 patients undergoing invasive nursing procedures and their family members were selected based on inclusion criteria and allocated randomly in three groups of 30 (with the presence of trained family members, with the presence of untrained family members and without the presence of family members) by minimization method. Inclusion criteria for patients were having informed consent to participate in the study, age 18-75 years, alertness and cognitive ability to answer questions, willingness for family members’ presence, inclusion criteria for family members also included being a close family member, being selected by the patient for bedside, having a desire to be with the patient, age 18-75 years, no history of aggressive bedside disease, no known mental illness and cognitive ability to respond There were questions. Exclusion criteria for the patient included worsening patient status and unwillingness to continue in the study. Exclusion criteria for family members were also intolerance to the end of the aggressive procedure and withdrawal from the study. Data collection tools included demographic information questionnaire of patients and family and Spielberger anxiety standard questionnaire. [23]. To conduct pre-test for patients in all three groups, the anxiety questionnaire was filled by face-to-face interview, then in the group of "patients with educated and present family" a family member selected by the patient and himself willing to attend, was briefed for 3-5 minutes about the procedure, and the conditions to be observed during the procedure. In the "Patients with educated family members" group, the intervention was performed only with the patient's family without any education. Family members of the third group also received no training, despite the desire to be with the patient, they were in the waiting room behind the door of the procedure room. Finally, immediately after the procedure, patients' anxiety was measured again in all three groups using the Spielberger questionnaire.
Research ethics standards such as receiving a code of ethics (Code of Ethics: IR.RUMS.REC.1396.166) and approval of the clinical trial registration system with code IRCT20180109038287N1 were obtained and informed consent was signed by the patient and family.
Data were analyzed by SPSS 16 software (SPSS Inc., Chicago, Ill., USA) at the significant level of 0.05 using Chi-square test (for comparison), Independent-sample Kruskal Wallis, paired t-test and ANOVA test.
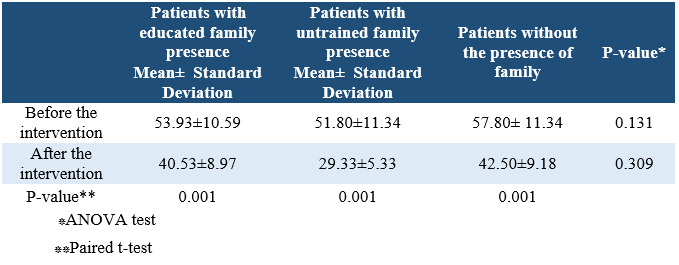
According to the results of the data analysis, the anxiety scores of the patients in the three groups after the intervention had a significant decrease compared to the pre-intervention phase. Based on the results of this study, the presence of family members and education before their presence could not have a significant effect on the level of anxiety in adult patients (Table 1).
Table 1. Comparison of mean and standard deviation of anxiety scores within and between study groups
In the literature review, there are limited studies on the impact of family members of adult patients on aggressive procedures during anxiety. Most studies focus on the presence of parents during cardiopulmonary resuscitation. Existing research has also reported conflicting results. Similar to our study in Işlekdemir et al., the presence of family members did not significantly affect the pain and anxiety of patients admitted to the emergency department undergoing aggressive nursing procedures [20]. While in a study by Kim, the presence of family members in the post-anesthesia care unit significantly reduced anxiety, delirium, and pain in patients, but did not affect the length of stay in the recovery room [21]. Hoseini Azizi et al. also reported that family support in the intensive care unit can accelerate the process of recovery for stroke patients [23]. Goldfarb et al., in a systematic review study, showed that although family-based and patient-centered care interventions in adult ICUs could not reduce mortality rates, they did produce positive outcomes such as reduced length of stay, reduced costs, and positive psychological experiences for the patient. And the family and their satisfaction increased. The researchers recommend high-quality empirical research to evaluate the effectiveness of family-based and patient-centered care in these areas [24].
However, the differences between recovery and adult care units and emergency departments in terms of the nature of hospitalized patients, physical environment conditions, and staff duties and responsibilities should not be overlooked. It seems to take on a different nature in sudden and unexpected situations such as hospital admissions, patient anxiety and family functioning. Researchers believe that the lack of documentary evidence justifies the necessity of family members being present in adult patients' bedside under invasive procedures [25]. Therefore, based on the available evidence, the presence or absence of family members cannot be properly weighted; therefore, it has been suggested that policymakers in each hospital should weigh the benefits and losses [26]. Literature review tells us that family presence, if necessary, and providing support during the experience of being present during aggressive procedures can have positive consequences for family, patient, and health workers [27].The findings of our study was not in line with aforementioned studies and according to the data obtained, attendance and education of family members could not reduce the anxiety of patients undergoing aggressive nursing procedures.
The presence of family members and receiving education before attendance could not reduce the anxiety of patients undergoing aggressive nursing procedures. Different aspects of the issue of family presence during aggressive procedures need to be addressed by researchers in future studies.
This article is the result of the Master's Degree in Internal Medicine and Surgery. The team would like to thank all the staff of Shahid Rahnemoon Hospital of Yazd University of Medical Sciences as well as all patients and their family members who contributed to this study. The Rafsanjan University of Medical Sciences Vice-Chancellor for Research has supported this research financially.
The authors declared no potential conflicts of interest regarding the research, authorship, and/or publication of this article.
Received: 2019/03/16 | Accepted: 2019/04/22 | Published: 2019/04/22
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






 gmail.com
gmail.com