BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://nmj.umsha.ac.ir/article-1-2097-en.html
2- Health
3- Midwifery Nursing ,
Multiple Sclerosis (MS) is the most common chronic disease of the central nervous system [1] and is spreading rapidly, affecting about 2.5 million people worldwide. In Iran, one in every 100,000 5.78 million people have MS [2]. Decreased sleep quality is a common complication in MS patients [8, 7]. Sleep disorders in patients with multiple sclerosis: insomnia, sleep apnea, restless legs syndrome, problem in falling asleep, inability to wake up and frequently wake ups. Sleep disorders can make a person feel tired, which can negatively affect a person's ability to do normal tasks during the day and can lead to excessive irritability [11-13, 8].
Research show that the involvement of various religious characteristics is associated with proper physiological function throughout the nervous system, hypothalamus, pituitary, adrenal, cardiovascular and immune systems [18].
According to the report, patients with MS have poor sleep quality, which greatly affects their quality of life and disease. Patients' spiritual needs also increase as the disease progresses. Nursing by nurses is a way to improve the condition of these patients. Due to the lack of research on the effect of spiritual care on the quality of sleep of MS patients, this study was conducted to determine the effect of spiritual care on the quality of sleep of patients with MS.
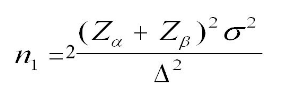
This is a semi-experimental study with two groups. The research society was all patients referring to the Association for the Support of MS Patients in Hamadan in 2018. Sample size according to Taheri et al.'s [22] study, assuming the first type of error was 1% and the test power was 90%, taking into account the minimum difference in size at 4 and standard deviation of 4 in the two-groups, through the following equivalent, 33 people were to be selected for each group; a 5% of drop was estimated for the sample size in each group, so 35 subjects were selected.
70 patients were selected from the patients referred to the Association for the Support of MS Patients who met the criteria to enter the research and had the desire to participate in the study. After identifying the samples, individuals were randomly assigned to the two experimental and control groups using random allocation software, so that each group was divided into 35 individuals. Criteria for entering the study included: 20 to 65 years of age, having Islam and Shiite religion, definitive diagnosis of MS according to a neurologist, level of disability between zero and 5.5 on the EDSS scale, poor sleep quality based on the Pittsburgh standard (High score 5) and not using sleeping pills. The criteria for leaving the study included: hospitalization of the patient due to recurrence of the disease, infection with other debilitating diseases, death of the patient during the research process and crisis in life such as: divorce and death of parents.
Data were collected through a demographic questionnaire and Pittsburgh Sleep Quality questionnaire. The intervention was held in the form of group meetings during the 4 weekly sessions of 45 to 60 minutes. Data were analyzed by SPSS 16 (SPSS Inc., Chicago, Ill., USA) and descriptive and inferential statistics (independent t-test and paired t-test).
There was no significant difference between the two groups in terms of demographic variables (P>0.05). There was no significant difference between the two groups before intervention in the sleep quality variable (P=0.678). There was a statistically significant difference between the two groups in the after-intervention-phase (P<0.001). Findings of the study showed the effectiveness of spiritual care on improving the quality of sleep in patients with multiple sclerosis. The results of the analysis are expressed in Tables 1, 2, 3 and 4.
Table 1. Comparison of groups in terms of quantitative variables
| P-value | df | t | M | SD | N | Group | Variable |
| 0.473 | 68 | 1.58 | 38.03 | 9.86 | 35 | Test | Age |
| 34.54 | 8.47 | 35 | Control | ||||
| 0.361 | 68 | 0.920 | 2.48 | 1.39 | 35 | Test | Diagnosis period |
| 2.23 | 0.94 | 35 | Control | ||||
| 0.398 | 68 | 0.852 | 2 | 1.11 | 35 | Test | Recurrences in one year |
| 2.20 | 0.83 | 35 | Control |
Table 2. Comparison of groups in terms of qualitative variables
| Group Variable |
Test group | Control Group | Fisher’s exact test | P-value | |||
| N | % | N | % | ||||
| Sex | Female |
30 |
85.7 |
25 |
71.4 |
3.884 | 0.133 |
| Male |
5 |
14.3 |
10 |
28.6 |
|||
| Marital status |
Single |
9 |
25.7 |
11 |
31.4 |
1.912 |
0.640 |
Married |
21 |
60 |
19 |
54.3 |
|||
Widower |
1 |
2.9 |
3 |
8.6 |
|||
Divorced |
4 |
11.4 |
2 |
5.7 |
|||
| Education |
Primary school |
5 |
14.3 |
2 |
5.7 |
2.696 |
0.803 |
High school |
3 |
8.6 |
6 |
17.1 |
|||
High school diploma |
15 |
42.9 |
14 |
40 |
|||
College |
3 |
8.6 |
4 |
11.4 |
|||
Post-Graduate |
8 |
22.9 |
8 |
22.9 |
|||
| Family support | Low | 5 | 14.3 | 1 | 2.9 | 7.532 | 0.055 |
| Medium | 10 | 28.6 | 9 | 25.7 | |||
| Good | 9 | 25.7 | 19 | 54.3 | |||
| High | 11 | 31.4 | 6 | 17.1 | |||
| Family history | Yes |
3 |
8.6 |
4 |
11.4 |
0.159 | 1.000 |
| No | 32 | 91.4 | 31 | 88.6 | |||
| Home situation |
Owning |
23 |
65.7 |
22 |
62.9 |
0.062 | 0.803 |
| Rental |
12 |
34.3 |
13 |
37.1 |
|||
| 7th area | 6th area | 5th area | 4th area | 3rd area | 2nd area | 1st area | Variable Time |
|
| M±SD | M±SD | M±SD | M±SD | M±SD | M±SD | M±SD | ||
| 0.76±1.34 | 0.87±0.69 | 0.51±1.51 | 1.29±1.43 | 1.03±1.60 | 0.97±1.77 | 0.66±1.74 | Test | Before Intervention |
| 0.53±1.11 | 1.04±1.03 | 0.24±1.06 | 1.30±1.14 | 1.11±1.69 | 0.80±2.11 | 0.72±1.69 | Control | |
| 0.151 | 0.139 | 0.001< | 0.361 | 0.739 | 0.111 | 0.729 | P value | |
| 0.48±0.66 | 0 | 0.24±0.94 | 1.22±1.26 | 0.86±0.83 | 0.61±0.74 | 0.48±0.66 | Test | After intervention |
| 0.53±1.11 | 1.02±1.20 | 0.28±1.09 | 1.27±1.03 | 1.11±1.69 | 0.80±2.11 | 0.71±1.69 | Control | |
| 0.001< | 0.001< | 0.001 | 0.446 | 0.001 | 0.001< | 0.001> | P value | |
Table 4. Average and standard deviation of the total score of sleep quality before and after the intervention in the two groups of test and control
| P-value | t | df | After intervention | Before intervention | Time Group |
| M±SD | M±SD | ||||
| 0.001> | 7.714 | 34 | 1.77±10.77 | 2.88±13.77 | Test |
| 0.136 | 1.528- | 34 | 2.17±13.69 | 2.24±51.13 | Control |
| 6.167- | 0.417 | t | |||
| 0.001> | 0.678 |
P-value | |||
The findings showed that before the spiritual care between the overall sleep quality of the patients in the experimental group (with average and standard deviation (13.77±2/88) with the overall sleep quality of the control group patients (with average and standard deviation (13.51±2.24) there is no significant statistical difference and they are homogeneous which was in line with the study of Taheri et al. [22]. Given that a total score of 5 or higher in the Pittsburgh Sleep Quality Questionnaire indicates poor sleep quality in patients [30], the findings showed that the quality of life of patients was low before the intervention, that were in accordance to research by Bahraini et al. [31], Najafi et al. [9], Jalalmanesh et al. [32], Motaharinezhad et al. [33], Lobentanz et al. [34], Braley. et al. [35], Kaminska et al. [36] and Fleming et al. [12].
Explaining these findings, we can understand the effect of spiritual beliefs in life as a factor in dealing with physical and mental problems caused by serious illnesses, so that spiritual care with an approach beyond and far from ordinary life to achieve peace and free from mental stress can also help improve health and sleep quality. Therefore, a comprehensive view of the patient's various dimensions can help the health care staff to provide better services to patients with chronic diseases, including MS. Since sampling is continuous in this research and the statistical population is selected only from among the members of the Association for the Support of MS Patients, it is recommended to conduct similar researches in Hamadan and other cities.
Regarding the effect of spiritual care on improving the quality of sleep, it is suggested that nurses and health care providers pay attention to the spiritual needs of patients and use spiritual care as a safe and cost effective way to improve patients' sleep.
This article is taken from the master's thesis of Internal Medicine Nursing, approved by Hamadan University of Medical Sciences, which is registered in the ethics committee of Hamadan University of Medical Sciences with the code IR.UMSHA.REC.1397.372. Researchers thank the Vice Chancellor for Research and Technology of the University for its financial support, the officials of the Association for the Support of MS Patients and the esteemed patients participating in this research.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Received: 2019/09/7 | Accepted: 2019/09/29 | Published: 2020/01/3
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






 gmail.com
gmail.com