BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://nmj.umsha.ac.ir/article-1-2214-en.html
2- Faculty member, Department of Psychiatric Nursing, School of Nursing and Midwifery, Qazvin University of Medical Sciences, Qazvin, Iran ,
3- M.Sc. Student, Department of Psychiatric Nursing, School of Nursing and Midwifery, Qazvin University of Medical Sciences, Qazvin, Iran
✅ Considering that EMDR, as a non- pharmacological intervention, reduced depression in patients with spinal cord injury.
Depression is the most common psychological consequences of spinal cord injury. There are several treatments for depression that are divided into two categories: pharmacological and non-pharmacological [17]. Medication almost doubles the chances of a depressed patient recovering within a month of taking the drug, but due to the side effects of these medications including drowsiness, insomnia, hypotension, cardiac arrhythmia, weight gain, anticholinergic side effects, dizziness, lethargy, ear discomfort, sexual dysfunction [17], the use of non-drug therapies has been considered more by scientists than ever before. Non-pharmacological treatments include eye movement desensitization and reprocessing (EMDR), a type of psychotherapy discovered in 1987 by Shapiro. This method helps to process and accelerate information by relieving the clogging of the information processing system by traumatic memories, and changes personality traits by transforming memories. Today, EMDR method is used in the treatment of many diseases, including depression, anxiety and stress [18]. This complex approach combines elements of behavioral and client-centered approaches in a way that claims that internal processes accelerate and facilitate psychological recovery. The success rate of this procedure, in one to three sessions or less, is between 90-84% depending on the severity of the trauma. The effectiveness of this method is higher than traditional therapies, which have a success rate of no more than 55% in 7-13 sessions and often last for years [19]. The purpose of this study was to determine the effect of eye movement desensitization and reprocess (EMDR) on depression in patients with spinal cord injury.
In this clinical trial study, 40 patients with Spinal cord injury (SCI) who were treated at Hadith Rehabilitation Center of Qazvin in 2018-2019 were selected by random sampling and randomly divided into two groups. The methods of eye movements and reprocessing were performed for experimental group in five sessions of 90 minutes. The research instruments included demographic characteristics form and Beck’s depression inventories that were completed by patients in both groups. Depression was measured before, one, three and six months after the intervention. Data were analyzed using SPSS 23 (SPSS Inc., Chicago, Ill., USA), by descriptive and inferential statistics proportional to the data. The data was analyzed with, Chi-square, independent t-test, Paired t-test and ANOVA.
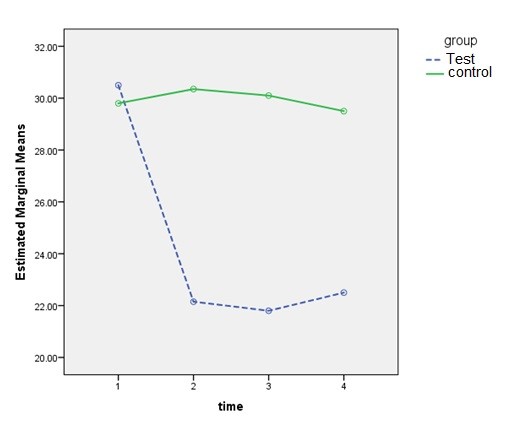
The results of this study showed that before intervention the mean depression score was not significantly different between the control and experimental groups (31.4 ±10.4), (30.5 ±6.3 ((P=0.7, t=-0.3). After intervention, the experimental group had a significant increase in the mean score of depression compared with the control group (22.3±7.7), (30.3±6.6) (P<0.001, t=-4.1. (The mean depression score in the experimental group showed statistically significant differences three and six months after the intervention (P=0.001, t=-4.05).
| Group Variable |
Test | Control | Independent t-test |
| M±SD | M±SD | ||
| Age | 34.6 ± 10.8 | 38.5 ± 13.2 | P=0.42 |
| Duration of illness (years) | 48 ± 9.2 | 47.02 ± 9.4 | P=0.65 |
| number of children | 22.4 ± 10.8 | 20.4 ± 9.9 | P=0.41 |
| marital status | N (%) | N (%) | Chi-square |
| Single | 12 (60) | 9 (45) | P=0.2=P |
| Married | 8 (40) | 11 (55) | |
| Female | 7 (35) | 4 (20) | P=0.29 |
| Man | 13 (65) | 16 (80) |
Table 2. Comparison of mean and standard deviation of patients' depression scores in experimental and control groups before, one, three and six months after intervention
| Group Follow-up |
Test (M±SD) |
Control (M±SD) |
Independent t-test |
| Before intervention | 30.5 ± 10.4 | 31.4 ± 6.3 | t=-0.3, P= 0.7 |
| 1 month after intervention | 22.1± 5.7 | 30.3 ± 6.6 | t=-4.1, P<0.001 |
| 3 months after the intervention | 21.8 ± 6.4 | 30.1 ± 7.5 | t=-3.7, P=0.001 |
| 6 months after the intervention | 22.5 ± 3.5 | 29.5 ± 6.9 | t=-4.05, P= 0.001 |
| Result of repeated analysis of variance test | F=11.29 P=0.001 |
F=1.13 P=0.34 |
According to the findings of this study, EMDR as a complementary and non-pharmacological treatment leads to a reduction in depression in patients with spinal cord injury. The results of this study are consistent with the findings of the study of Khazaeipour et al. [27]. The results of the study of Mokhber Dezfoly et al. [28], Krause et al. [29], Hancock et al. [30] and Hatefi et al. [31] also confirm the results of this study. EMDR was able to reduce depressive symptoms in a follow-up period of one, three and six months after intervention in patients with spinal cord injury. Accordingly, the study of Ostacoli et al., which shows that this treatment can be complementary to drug therapy and improve depression in patients, is consistent with the findings of this study [20]. In addition, the results of Wood et al.'s research showed that most people treated with EMDR had a significant improvement and this method can be a good treatment for recurrent or long-term depression in people with post-stroke depression [21]. These results are consistent with the findings of this study. Gauhar's findings also showed an improvement in depressive symptoms and quality of life and its persistence in the trimester after treatment [22]. Hofmann et al. also found that patients who received EMDR treatment in addition to cognitive-behavioral therapy had a greater improvement than patients who received only cognitive-behavioral therapy [23]. Hase et al. also showed that EMDR treatment improves depression in treated patients and they had less problems and recurrence during the one-year follow-up period [24]. The results of the study by Malandrone et al. confirmed the findings of the present study [32]. The limited number of samples in this study as well as conducting this study in a rehabilitation center may be one of the limitations of the study that needs to be observed in generalizing the results as a precaution.
The results of this study confirmed that EMDR method is effective in treating and reducing depression scores in patients with spinal cord injury who have depressive symptoms. These results persist for three to six months after the intervention and can be used as a non-pharmacological, complementary and effective method in the treatment of depression in patients with spinal cord injury. For more generalizability of the results of this study, it is suggested that in future studies, citing the results of this study, this method be widely considered as a complement to various medical and non-pharmacological treatments in patients with depressive symptoms.
Respected authorities of the Welfare Organization and Hadith Spinal Cord Injury Center in Qazvin Province and all patients with spinal cord injury are thanked as participants in this study.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Received: 2020/04/18 | Accepted: 2020/07/24 | Published: 2020/10/11
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






 gmail.com
gmail.com